
Introduction
Miscarriage is a heartbreaking experience no one ever wants to face, let alone more than once. But for some, it’s a devastating reality. When a woman experiences multiple miscarriages, doctors refer to it as recurrent abortion or recurrent pregnancy loss (RPL). While it’s emotionally exhausting, it’s not the end of the road. Understanding the causes, risks, and treatment options is the first step toward hope and healing.
Understanding Recurrent Abortion
Medical Definition
Recurrent abortion is typically defined as the loss of two or more consecutive pregnancies before the 20th week of gestation. Some medical guidelines, such as those from the American Society for Reproductive Medicine (ASRM), consider three or more consecutive losses as the threshold. Either way, recurrent miscarriage is a red flag that needs medical attention.
Difference Between Recurrent and Single Miscarriage
A one-time miscarriage is, sadly, common—affecting up to 15% of pregnancies. But recurrent abortions suggest an underlying issue, whether genetic, hormonal, anatomical, or otherwise. Unlike a single miscarriage, recurrent miscarriage triggers a deeper diagnostic approach.
Causes of Recurrent Abortion
Understanding the “why” behind pregnancy losses can feel like putting together a puzzle. Let’s break down the main culprits.
Genetic Causes
About 2-5% of couples experiencing recurrent abortion carry a genetic abnormality, usually a balanced translocation. This means part of a chromosome has switched places with another but without losing any material—yet it can cause unviable embryos.
Anatomical Abnormalities
Some women are born with uterine anomalies, such as a septate uterus, bicornuate uterus, or fibroids. These can prevent a fetus from implanting or growing properly.
Hormonal Imbalances
Conditions like thyroid disorders or polycystic ovary syndrome (PCOS) can lead to hormone irregularities that interfere with the uterine lining and fetal development.
Immunological Factors
Autoimmune issues like antiphospholipid syndrome (APS) can cause the immune system to attack the embryo or form blood clots that interfere with placenta formation.
Infections
Certain infections, especially those caused by listeria, toxoplasmosis, or cytomegalovirus, can lead to early pregnancy loss if untreated.
Lifestyle and Environmental Factors
Smoking, excessive alcohol, drug use, obesity, and even exposure to environmental toxins can increase miscarriage risks.
Risk Factors

Maternal Age
Women over 35 face higher chances of miscarriage due to age-related chromosomal issues.
Paternal Factors
While often overlooked, the age and health of the male partner—including sperm quality—can play a role.
Previous Pregnancy Complications
Having had previous stillbirths, miscarriages, or pregnancy complications increases your risk of recurrent loss.
Symptoms and Warning Signs
Physical Symptoms
- Vaginal bleeding
- Cramping or abdominal pain
- Fluid or tissue passing from the vagina
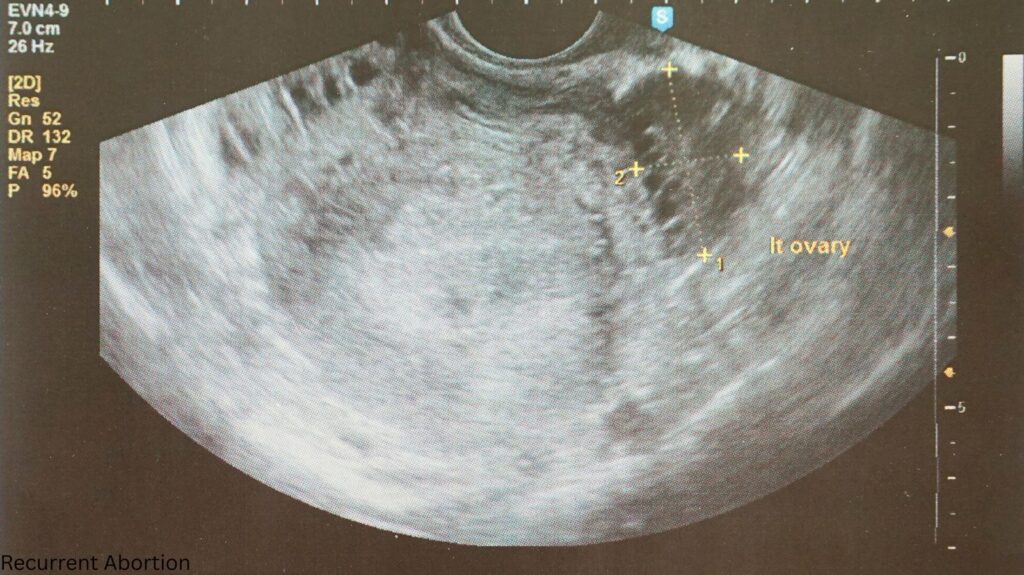
However, not all miscarriages come with noticeable symptoms, especially missed abortions detected only via ultrasound.
Emotional and Mental Health Impact
The grief is profound. Anxiety, depression, and PTSD are not uncommon. Recurrent miscarriage is not just a physical issue—it’s a deeply emotional one.
Diagnostic Process
Getting answers is crucial, and it starts with thorough testing.
Blood Tests
- Hormone levels
- Clotting disorders
- Autoimmune markers
Imaging and Scans
- Ultrasounds
- MRI or hysteroscopy to check the uterus’ structure
Genetic Testing
Karyotyping for both partners may reveal chromosomal issues.
Hormonal Assessments
Thyroid function and progesterone levels are key metrics.
Treatment and Management Options

There’s hope—plenty of it.
Medications
- Blood thinners for clotting disorders
- Progesterone supplements
- Thyroid hormone replacement
Surgical Treatments
Corrective surgeries can fix uterine anomalies or remove fibroids.
Lifestyle Modifications
Quitting smoking, eating healthy, maintaining a healthy weight, and managing stress are essential steps.
Psychological Support
Therapy or support groups can help couples process grief and move forward with resilience.
Coping Emotionally with Recurrent Miscarriage
The Emotional Rollercoaster
You’re not just losing a pregnancy—you’re losing dreams, hope, and stability. It’s okay to grieve and not be okay.
Therapy and Counseling
Licensed therapists specializing in pregnancy loss can help navigate this storm. Some couples also benefit from couples therapy or spiritual counseling.
When to See a Specialist
If you’ve had two or more miscarriages, don’t wait—consult a reproductive endocrinologist or fertility specialist. Early evaluation improves your chances of a healthy pregnancy.
Recurrent Abortion in India and Globally
Awareness and Access to Care
In India and many other countries, limited awareness and access to specialists delay diagnosis. Thankfully, urban healthcare is catching up.
Cultural Stigma
Sadly, many women are blamed, shamed, or misunderstood. Educating society and empowering women is key to fighting this stigma.
Myths vs. Facts About Recurrent Abortion
- Myth: You did something wrong.
Fact: Most causes are medical—not your fault. - Myth: You can never have children.
Fact: Many women go on to have healthy pregnancies after treatment. - Myth: It’s only a women’s issue.
Fact: Male partners can contribute to miscarriages too.
Conclusion
Recurrent abortion is tough—physically, emotionally, and spiritually. But it’s not the end of your story. With the right medical support, emotional care, and persistence, there’s a real chance to achieve a healthy pregnancy. The journey may be rocky, but it’s not without hope.
FAQs
1. Can stress cause recurrent abortion?
Chronic stress may contribute indirectly by affecting hormones and immunity, but it’s rarely the sole cause.
2. Is there a cure for recurrent abortion?
It depends on the cause. Many medical conditions can be treated or managed effectively.
3. How soon can you try again after a miscarriage?
Physically, you can try again after 1–2 menstrual cycles, but emotionally, give yourself time to heal.
4. Can lifestyle changes really help?
Yes! Quitting smoking, eating well, exercising, and managing stress can significantly improve outcomes.
5. Are recurrent abortions hereditary?
Some genetic factors may be inherited, but many causes are non-genetic and treatable.

